Download this report or read online:
- Assisted Dying Service yearly report 2022/2023 (DOCX 172KB), (PDF 304KB)
The second Annual Service report reflects a summary of individuals’ interactions with the Assisted Dying Service between 7 November 2022 – 31 December 2023. Importantly, this year’s report includes 13 months, to align future reports with the calendar year for better comparison and an improved reporting structure. Note that some applications received during this time were ongoing at the end of the reporting period.
A more detailed report for data across the first year of service (November 2021 - November 2022) can be found on Health New Zealand | Te Whatu Ora website: Assisted Dying Service yearly report 2021/2022 (Word Version), (PDF Version).
Assisted dying involves a person experiencing unbearable suffering from a terminal illness taking or being administered medication to end their life. There are strict eligibility criteria to have an assisted death. Not everyone with a terminal illness will be eligible. New Zealanders aged 18 or over who have a terminal illness which is likely to end their life within 6 months may be able to access assisted dying.
The service involves specific steps, medical assessments, and essential safeguards. These are to ensure a person is eligible and making their decision independently, without pressure from anyone. The framework for the service and its eligibility criteria and safeguards are set out in the law, called the End of Life Choice Act 2019 (the Act). The Assisted Dying Service is overseen by the Ministry of Health | Manatū Hauora.
The information routinely collected by Health New Zealand | Te Whatu Ora is determined by the requirements outlined in the Act. This report follows the specific purpose of gathering and reviewing information as mandated within the Act. The content included within this report is presented in the interest of both public and academic review.
Within the document, we use the acronyms AMP (referring to attending medical practitioner) and IMP (referring to independent medical practitioner). These practitioners perform the medical assessments to determine eligibility. For more information relating to practitioner roles, please refer to our website or the End of Life Choice Act 2019.
Certain low numbers relating to applications within the year review are enclosed in full. The decision to disclose this information is made in specific instances with explicit consideration of the protection of privacy of those involved. To protect the privacy of the patients, whanau, and medical practitioners involved with the service, some information has been suppressed.
Overview of assisted dying applications
Between 7 November 2022 and 31 December 2023, Health NZ received 1015 formal applications for assisted dying. Of these 1015 applications 978 have progressed from initial application to AMP assessment. Those 37 who did not progress either:
- withdrew their application
- died before the AMP assessment was formally initiated
- were found to be ineligible prior to formal initiation of the AMP assessment
- the application was still open (had not yet progressed to assessment) during the period set out in this report.
Over this reporting period, AMPs completed 1041 assessments and IMPs completed 768 assessments. These are inclusive of assessments completed for open applications carried over from previous period. Of those assessed over the year, 624 applications were confirmed as eligible and 396 assisted deaths occurred. During this period, 584 applications did not proceed to an assisted death following assessment due to:
- the applicant withdrawing their application
- the applicant being found ineligible or not competent to give consent at or following assessment
- the applicant dying as a result of underlying conditions
- the application being found to not comply with the Act at final review.
Figure 1 below outlines the number of applications initiated per month during this period. Note that November 2022 in Figure 1 reflect a partial month from 7 November 2022.
Figure 1: New applications received by month
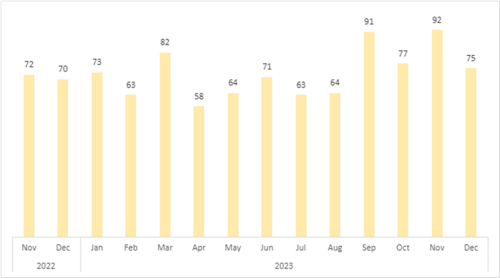
Table 1: Demographic summary of new applications
Of the 1015 new applications received over the year:
- 82% were NZ European/Pākehā
- 4% were Māori
- 48% were Female/Wāhine; 52% Male/ Tane
- 79% were 65 years or older
- 75% were receiving palliative care at the time of the application
- 67% had a diagnosis of cancer.
| Demographic summary: New Applications (N= 1015) 7 November 2022 – 31 December 2023 |
Number of people3 |
% of applications |
|
|
Ethnic group1 |
Māori |
44 |
4.33% |
|
Pacifica |
7 |
0.69% |
|
|
NZ European/Pākehā |
835 |
82.27% |
|
|
Asian |
23 |
2.27% |
|
|
Other |
125 |
12.32% |
|
|
Sex |
Female/Wāhine |
492 |
48.47% |
|
Male/Tāne |
523 |
51.53% |
|
|
Gender diverse |
0 |
0 |
|
|
Age group |
18-44 years |
18 |
1.77% |
|
45-64 years |
193 |
19.01% |
|
|
65-84 years |
601 |
59.21% |
|
|
85+ years |
203 |
20.00% |
|
|
Diagnosis2 |
Cancer |
684 |
67.39% |
|
Neurological condition |
92 |
9.06% |
|
|
Chronic Respiratory Disease |
53 |
5.22% |
|
|
Cardio-Vascular condition |
60 |
5.91% |
|
|
Other organ failure |
24 |
2.36% |
|
|
Multiple Co-Morbidities |
45 |
4.43% |
|
|
Not known4 |
130 |
12.81% |
|
|
Receiving palliative care at time of application? |
Yes |
764 |
75.27% |
|
No |
251 |
24.73% |
|
|
Reported a disability at time of application? |
Yes |
140 |
11.76% |
|
No |
875 |
88.24% |
Notes:
- Total ethnicity has been used. This means that individuals reporting more than one ethnicity are included within each category to which they identify. In the current report, individual identification as ‘European’ has been included within the ‘Other’ category, distinct from NZ European/Pākehā
- Total diagnosis has been used. This means that individuals presenting with multiple diagnoses are included within each applicable diagnostic category.
- Repeat applications are included as unique instances. This means that in cases where an individual submits multiple applications during this period, their information is recorded in the demographic data each time.
- ‘Diagnosis not known’ includes individuals who have applied but have not yet completed their first assessment with their AMP, as well as those who have withdrawn before assessment, died before this assessment was completed, or were ineligible due to not having a terminal illness.
Applications received by location
Table 2 provides a summary of formal applications by location for the review period (7 November 2022 – 31 December 2023). We have included a summary relating to both the historical DHB (district health board) system, as well as the new observed Health New Zealand regions.
Table 2: New applications by location
|
Region |
Locations included |
Number of applications |
Percentage of total applications |
|
Northern
|
Auckland |
281 |
32.71% |
|
Northland |
51 |
||
|
Te Manawa Taki (Midland)
|
Bay of Plenty |
109 |
24.14% |
|
Gisborne |
6 |
||
|
Taranaki |
21 |
||
|
Waikato |
109 |
||
|
|
|||
|
Central
|
Hawke's Bay |
43 |
19.9% |
|
Manawatu-Wanganui |
38 |
||
|
Wellington |
121 |
||
|
|
|||
|
|
|||
|
|
|||
|
Te Waipounamu (Southern)
|
Canterbury |
107 |
23.25% |
|
Marlborough |
15 |
||
|
Nelson |
30 |
||
|
Otago |
33 |
||
|
Southland |
23 |
||
|
Tasman |
13 |
||
|
West Coast |
15 |
Assessments completed during this period
After an application is submitted, an initial assessment is made by an AMP. This practitioner reviews eligibility against the criteria as outlined in the Act. The IMP provides an independent second assessment. Go to Commonly used terms in the Assisted Dying Service for more information relating to practitioner roles, or the End of Life Choice Act 2019.
Applications may be found ineligible at each of these assessments for a variety of reasons. For more information on ineligibility outcomes at assessment for this first year of service please see Table 4.
Following eligible outcomes at both AMP and IMP assessments, AMPs meet with the applicant for further discussion relating to eligibility and the assisted dying process. At this time, some previously eligible applicants may be found no longer competent to continue. This outcome occurred 3 times between 7 November 2022 to 31 December 2023.
Table 3 outlines the number of assessments undertaken, and the associated outcomes, at each stage of the assisted dying process.
Table 3: Assessment outcomes
|
|
Outcome of assessment |
Number of assessments |
|
AMP Assessments (N = 1041) |
Eligible |
862 |
|
Ineligible |
179 |
|
|
IMP Assessments (N = 768) |
Eligible |
748 |
|
Ineligible |
20 |
|
|
Eligibility Discussion Following Assessment (N = 627) |
Eligible |
624 |
|
Ineligible |
3 |
Note: The number of assessments in Table 3 are inclusive of applications that were open and carried over from the previous period.
Reasons to be found ineligible at AMP and IMP stage
Not all applications made to the Assisted Dying Service will result in an assisted death; some individuals may be assessed as ineligible. Reasons for ineligibility vary, and may relate to an applicant’s age, status as a New Zealand citizen/resident, or considerations relating to their health and physical decline. For more information about eligibility criteria, please refer to our website.
Table 4 outlines a summary of ineligibility decisions at each stage of assessment by AMP and IMPs (referred to in Table 3). Being found eligible at AMP assessment stage and ineligible at IMP assessment stage may occur due to a number of reasons, including but not limited to a change in personal circumstances impacting eligibility and/or a change in prognosis.
Table 4: Ineligibility summaries: Assessed by AMP and IMP
|
The applicant is… |
Ineligible at AMP assessment (179) |
Ineligible at IMP assessment (20) |
|
Not a New Zealand Citizen/Permanent resident |
7 |
0 |
|
Not aged 18 or over |
0 |
0 |
|
Not experiencing unbearable suffering in a manner that the person considers tolerable |
77 |
9 |
|
Not in an advanced state of irreversible physical decline |
79 |
4 |
|
Not suffering from a terminal illness that is likely to end their life within 6 months |
133 |
10 |
Note:Total reasons for ineligibility have been applied. This means that individuals may be found to be ineligible across multiple criteria, and each observed reason is included in the report.
Assessed applications not continuing to Assisted Dying
Table 5 summarises applications where an assessment had occurred (at AMP or IMP), but the applicant had not progressed to an assisted death. This table specifically relates to applications not accounted for as ineligible at the AMP or IMP assessments (as per Table 3). Additionally, this table includes applications which are still open at the time of review and are therefore not associated with a known outcome.
There are several reasons why an individual may not continue their application to an assisted death. These include being found ineligible following a prior eligible outcome or becoming unable to make an informed decision/give consent. Individuals may also withdraw their application or die of an underlying condition/terminal illness at any point during the application process or before their scheduled assisted death. Furthermore, individual applications may be found non-compliant with the Act during final review before an assisted death may occur.
Table 5: Application not progressed to an assisted death
|
|
Number of assessments |
|
Died in process |
307 |
|
Lost competence |
53 |
|
Lost eligibility |
13 |
|
Decided to withdraw |
55 |
|
Application found to be not compliant with the Act at final review |
2 |
|
Application is still open at the time of review |
27 |
Requested competence assessment
In some situations, a person will also be seen by a psychiatrist. This will happen if the AMP and IMP both think the person is eligible, but one or both have concerns about whether the person is competent to make an informed decision.
During the period described, only 12 individuals were referred for a competence assessment. All but two were determined to be competent to consent, while the remaining individual died in process before a decision had been completed.
Number of re-applications
94 individuals made more than one application for an assisted death during the reporting period. There are several reasons why an individual might make more than one request. This includes, but is not limited to:
- the applicant being assessed as ineligible at the time of the first application, and choosing to reapply
- the applicant withdrawing their original request and then deciding to reapply
- an observed change in the applicant’s individual circumstances which affects their eligibility (e.g., a change in prognosis).
No individual has made more than one reapplication during this reporting period.
Assisted deaths
Number of assisted deaths
Between 7 November 2022 and 31 December 2023, 396 people had an assisted death.
The figure below outlines the number of applications initiated, eligible applications following assessment (referred to in Table 3), and assisted deaths by month. Note that November 2022 in Figure 2 reflects a partial month (from 7 November 2022 to 30 November 2022).
Figure 2: Application and eligibility of assisted deaths
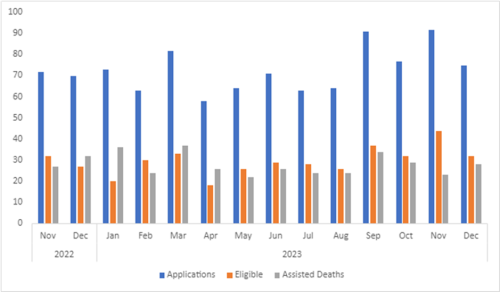
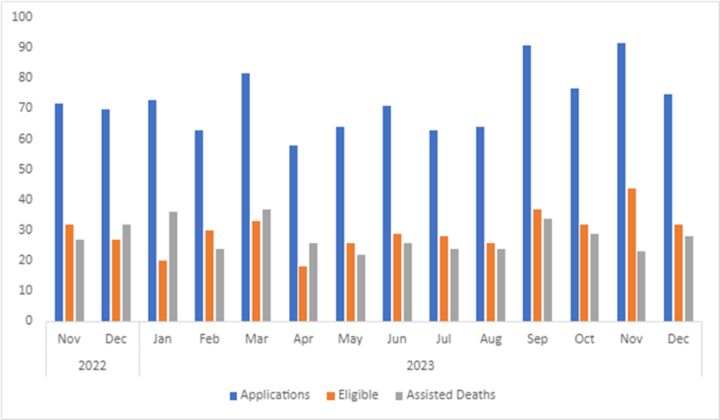
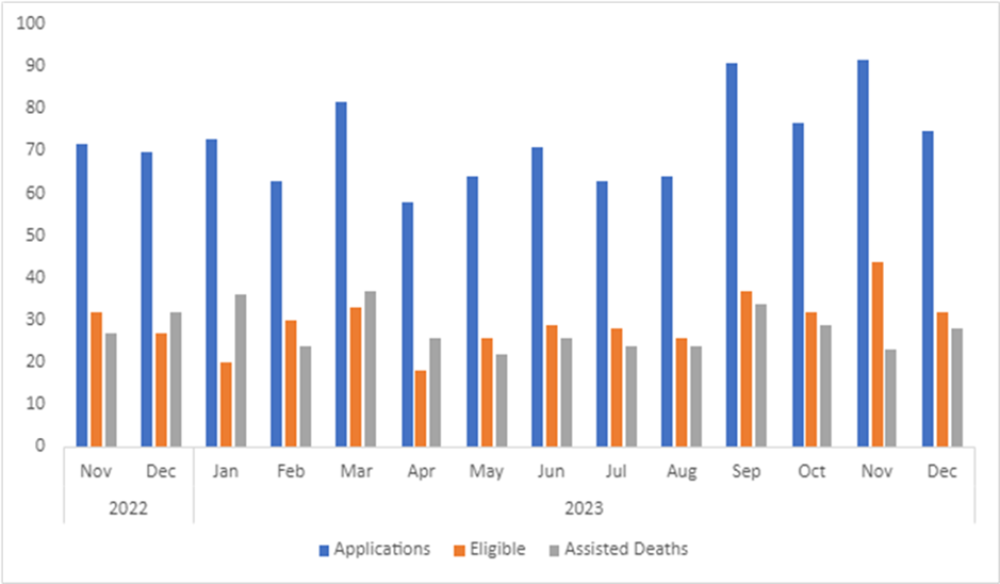
Figure 2: Application and eligibility of assisted deaths
Location of assisted deaths
Assisted deaths can take place at the person’s home, in hospital, or in the community. The summary by location for this period of review is:
- 321 (or 81.1%) at the person’s home or another private property
- 31 (or 7.8%) in a public hospital
- 34 (or 8.6%) in an aged care facility
- 10 (or 2.5%) in a hospice facility.
SCENZ Group practitioner lists
The Support and Consultation for End of Life in New Zealand group (SCENZ group) is responsible for maintaining the list of medical practitioners and Psychiatrists involved in providing assisted dying services. As of the date of review, there were 127 practitioners registered as members on the SCENZ list.
Medical practitioners can be on the SCENZ list for more than one role, depending on their scope of practice (AMP, IMP, Psychiatrist). The SCENZ group also holds a list of willing Nurse Practitioners. For more information about the SCENZ group and practitioner roles, please refer to our website.
Table 6 outlines the number of each role on the SCENZ list, by region. Due to low numbers, precise numbers by region of Nurse Practitioners (total = 13) and Psychiatrists (total = 10) are suppressed.
More than half of all practitioners (AMP, IMP, Nurse Practitioners, and Psychiatrists) have indicated that they are willing to travel to facilitate access to the service.
Table 6: Health practitioner by location
|
|
Primary Location |
|
|||
|
|
Northern |
Midland |
Central |
Southern |
Willing to Travel |
|
AMP (88) |
25 |
15 |
17 |
31 |
45 |
|
IMP (80) |
23 |
18 |
13 |
26 |
44 |
|
Both AMP and IMP* (64) |
18 |
13 |
12 |
21 |
36 |
|
Nurse Practitioner (13) |
S |
S |
S |
S |
5 |
|
Psychiatrist (10) |
S |
S |
S |
S |
4 |
Notes
*In the case of AMP and IMP, practitioners may choose to perform either, or both, of the roles. In this reporting, ‘Both AMP and IMP’ reflects a practitioner who performs both roles. Practitioners performing both roles are also represented within the respective totals included above (i.e., AMP 88; IMP 80).
A growing number of health practitioners have chosen to provide services as an AMP for their own patients without registering to be included as a SCENZ member. A portion of these health practitioners have subsequently chosen to join the SCENZ group, and to make themselves available to additional patients.
Assisted Dying Education
During 2023, the assisted dying Service team presented to the topic of Assisted Dying on 21 occasions. The majority of groups requesting education about Assisted Dying were Health practitioners, both in hospitals in in the community during conferences and study days.
During this engagement, the team spoken to approximately 1150 people about assisted dying.
Disclaimer
An earlier version of this quarterly report was published with a validation error. The report has since been corrected as of 13 November 2024 to remove duplicate applications.